Borderline Personality Disorder (BPD) is a complex mental health condition characterized by intense mood swings, unstable relationships, and difficulties with self-identity. When combined with addiction, the challenges can become even more profound. In this blog, we’ll delve into the connection between Borderline Personality Disorder and addiction, explore the unique treatment considerations for individuals facing both conditions, and highlight the importance of integrated care.
Understanding Borderline Personality Disorder
Borderline Personality Disorder is characterized by a pervasive pattern of instability in mood, interpersonal relationships, self-image, and behavior. Individuals with BPD often experience intense emotional reactions, rapid mood shifts, fear of abandonment, and difficulties with impulse control. These emotional challenges can contribute to a higher risk of engaging in substance abuse as a way to cope with overwhelming feelings.
The Link Between BPD and Addiction
The link between Borderline Personality Disorder and addiction is complex and bidirectional. Individuals with BPD may be more susceptible to substance abuse as a way to alleviate emotional pain, regulate mood, or numb distressing feelings. Conversely, substance abuse can exacerbate the symptoms of BPD, intensifying mood swings, impulsivity, and relationship difficulties.
Integrated Treatment Approach
Effective treatment for individuals with Borderline Personality Disorder and addiction requires an integrated approach that addresses both conditions simultaneously. Treating one without the other can lead to incomplete recovery and a higher risk of relapse. Here’s how an integrated treatment approach can make a difference:
- Comprehensive Assessment: A thorough assessment by mental health professionals is essential to identify the presence of both BPD and addiction. This assessment informs the development of a personalized treatment plan that addresses the unique needs of each individual.
- Dialectical Behavior Therapy (DBT): DBT is a highly effective therapeutic approach for individuals with BPD. It focuses on developing mindfulness, emotion regulation, interpersonal effectiveness, and distress tolerance skills. DBT can help individuals manage intense emotions without resorting to substance abuse.
- Dual Diagnosis Treatment: Dual diagnosis treatment programs are designed to address co-occurring mental health disorders and substance use disorders. These programs offer a holistic approach that combines therapy, counseling, medication management, and support groups.
- Cognitive-Behavioral Therapy (CBT): CBT can be beneficial for addressing the thought patterns and beliefs that contribute to addictive behaviors. It helps individuals develop healthier coping mechanisms and replace negative thought patterns with more adaptive ones.
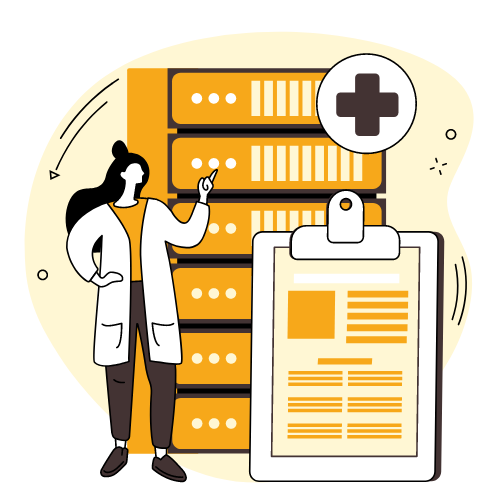
- Medication Management: In some cases, medications may be prescribed to manage the symptoms of BPD and support addiction recovery. These medications are typically used in combination with therapy and counseling.
- Supportive Environment: Creating a supportive and understanding environment is crucial for individuals with BPD and addiction. Family therapy and involving loved ones in the treatment process can contribute to a more stable and conducive recovery journey.
- Relapse Prevention: Individuals with BPD and addiction are at a higher risk of relapse due to the complexity of their conditions. A comprehensive relapse prevention plan should be an integral part of their treatment, focusing on coping strategies and early intervention.
- Long-Term Follow-Up: Continuing care and ongoing support are vital for maintaining recovery. Regular therapy sessions, support groups, and monitoring by mental health professionals help prevent relapse and ensure sustained well-being.
Borderline Personality Disorder and addiction create a unique set of challenges that require a specialized and integrated treatment approach. Treating both conditions concurrently through therapies like DBT and CBT, medication management, and support from mental health professionals can significantly improve the chances of lasting recovery. The intersection of BPD and addiction requires compassion, understanding, and a commitment to addressing the underlying factors contributing to both conditions. With the right treatment, individuals can achieve a more stable and fulfilling life free from the grip of addiction and the challenges of BPD.